“Wow. That is a lot of blood.”
Now, to be honest, this may have been a masturbation-related injury.
I caught COVID-19. I had traveled to Florida and family convinced me to go to Disney. I had all four shots: initial Pfizer, Pfizer first booster, Moderna second booster. I tried to mask reliably, but one still has to eat, and I felt safer outdoors; I shouldn’t have, but I did, so I took it off when outside. There were still too many people, too many crowds.
And so I caught it, probably BA.5 or BA.2.75. I isolated in my hotel room, now in Fort Lauderdale, and got a prescription for Paxlovid, and was doing okay. Not great– every swallow felt like I was gargling broken glass mixed with thumb tacks– but okay. Omaha had gotten another room to isolate away from me, and the hotel was being more than accomodating. The morning desk person was terrible, tried to kick me out even though Omaha had negotiated with the manager for the extension; but after calling the manager not only did we get the extension, but they left us plastic bags of their complimentary Continental breakfast (oranges and four cups of yogurt) at our door. So everything seemed under control.
But I was
bored. And you know, when a healthy man is bored, and there’s nothing on TV, he, er, takes to stroking his, er, boredom away. So I did. And I hadn’t gotten anywhere yet when I felt this sharp pain in my gut. So, I stopped. Awhile later (like, a whole movie later–
Free Guy, great film, I want to watch it again as I missed the first 45 minutes or so), I realized I hadn’t had much food or water that day, and the disease makes you sweat like Alex Jones facing judgment, so I got up and filled my one-liter bottle from the tap. I drank about a quarter of it, still didn’t feel great, got into the shower since showers are my go-to source of warmth, isolation, and white noise comfort. I realized that wasn’t making me feel any better, so I turned off the shower.
You know those 80s video games, the arcade ones where the display’s memory is just part of all the memory on the motherboard? When the game boots up, it needs that memory for other things, so the screen is scrambly and weird until it hooks into position zero of the game’s program counter and behaves correctly. I was suddenly kinda like that.
My mind was a very dark grey, almost black, the threads of thought random and colored dark red. The narrative that is
Elf started to cohere, the threads grew thicker and bundled together, and I opened my eyes. I don’t remember questioning why I was on the floor. But it was wet and cold, and I moved to turn over and my hand splashed in… red.
Blood?
“Wow. That is a lot of blood.”
I stood up– pulled myself up, using the countertop, really– looked at myself in the bathroom mirror. I knew where I was and who I was, but that guy in the mirror had the widest staring eyes I’ve ever had. There was blood in my hair and all down the right side of my face. There was blood on my chest. I was naked, wet, and cold. “Wow,” I said. “That is a lot of blood.” I looked under the counter and, yeah, there was a lot of blood, a puddle at least 30cm in diameter, ringed in water from my wet body. Naked and bloody, I stumbled into the bedroom, found the phone, realized I couldn’t read the instructions, stumbled to the bed, found my glasses, got back to the phone. “Hi, uh, I just woke up in a pool of my own blood. Could you call me an ambulance?”
“Oh! Uh, yeah, sure. Room 511, right?”
“Yeah.” I hung up, then found my cell phone and called Omaha. “Honey? I just asked the front desk to call me an ambulance. I just woke up in a pool of my own blood.”
“I’m coming over there!”
She did. She found me on the bed. She answered the phone, and took advice from the paramedic on the way about how to stop my nose from bleeding so much. The paramedics arrived and began asking me questions, which I answered competently. I knew my name, date of birth, address of record, and so forth. I could still quote Shakespeare. (It’s Marvel canon that whenever Tony Stark suffers from a concussion, he recites the ending of Hamlet, Act 2, Scene 2, that whole “For the Devil hath power to assume pleasing shape…” speech, to make sure his brain is still in working order.) Sheriffs arrived and determined it was not a crime scene. The paramedic asked, “Do you want to go to the hospital?”
“Hell, yes.”
“Let’s go.”
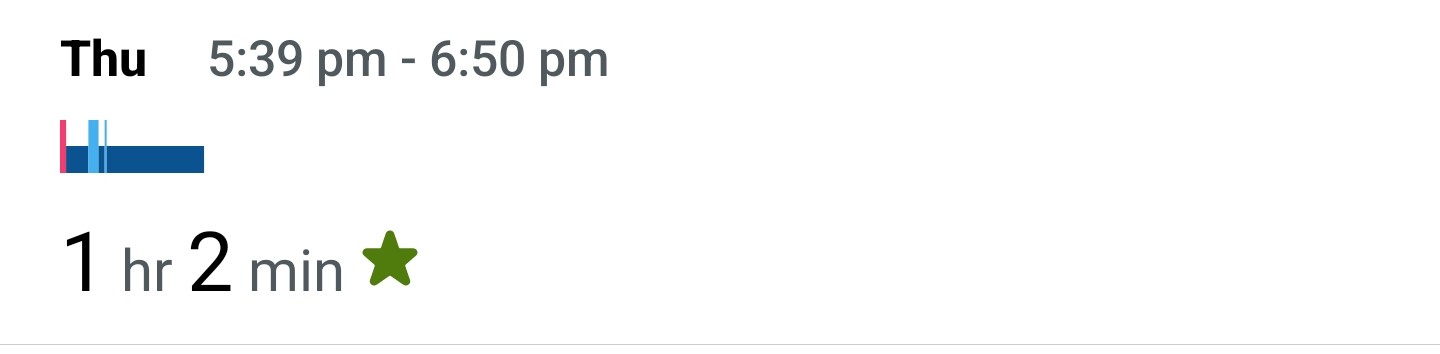
A reconstruction of the incident now includes one relevant detail: I was on that floor, unconscious, for an hour and eleven minutes. That’s what the Fitbit says; I was still and unmoving from 5:39pm until 6:50pm. I count myself lucky to be alive, to have come to at all.
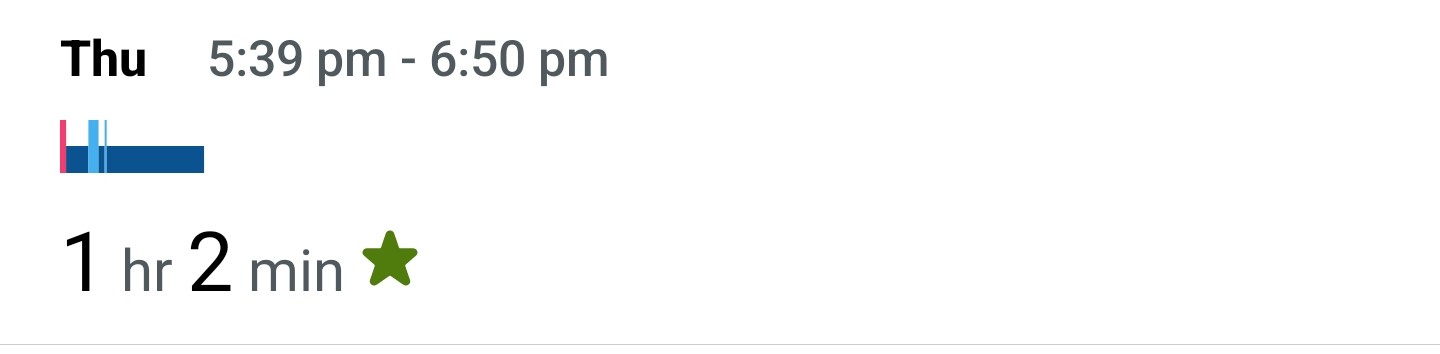 One hour, 11 minutes
One hour, 11 minutes
While we were at the hospital, I was seen by another sheriff who wanted to check the story. When I got to the point about not masking when outdoors at Disney, he snorted and said, “You gotta live your life.” My life is sexy, academic, athletic, and somewhat internal. I live a lot in my own head. Disney was a high risk, and I shouldn’t have done it. There’s not even a viable Truvada for COVID.
At the hospital there were no trauma rooms, so I was left on a gurney in a hallway. I complained about neck pain and was immediately put into a neck brace. Annoying. I met my admitting nurse, who was relentlessly cheerful, Jamaican, adorably hot, and competent as hell. She sent me to a CAT scan, where…
We discovered that I had hemorrhaging and blood in my peritoneal cavity, but my temperature was stable so there wasn’t peritonitis or sepsis. That pain I had felt was COVID shattering blood vessels in my abdomen. Not only was there a lot of my blood loose on the hotel bathroom floor, there was a lot of blood loose and sloshing around in the space around my intestines. I was immediately admitted and a battery of tests were conducted.
The good news, such as it was, is that my hemoglobin levels stabilized almost immediately; my body had recognized the damage and clotted quickly, starting the healing process.
I probed: A cut on my scalp, but very small. The left nostril had been bleeding freely, the right less so. The most damage was a laceration on the inside of my lip, a deep and wide self-inflicted bite wound when I fell. A doctor showed up and gave me very painful injections of lidocaine in the lip, followed by three stitches that he said “Have to be looser than normal so the wound drains properly. The mouth has the most germs of any place, even your backside.” Somehow (“Somehow?” C’mon, Elf) I knew that already. But he was both kind and hella competent, and sewed me right up. As he did, someone in the ER started playing “When the Saints Go Marching In” on a harmonica and… it was kinda nice, actually?
The ER Trauma surgeon, one of those tall, thin, early 30-somethings that
I am more than okay with born psychopaths being surgeons. They get to be well-paid, lauded as heroes, love the challenges, and have no hesitation to cut into people to show off those hard-earned skills.
radiates with health and competence, listened to my story, shook his head with a little smile, said “Fucking COVID” as if it had brought him fascinating new problems, and then gave that little laugh only born psychopaths are capable of. I’ve known a few. This guy was totally in the mold.
 Battered, bruised, bleeding internally, happy to be alive.
Battered, bruised, bleeding internally, happy to be alive.Somewhere in there, Omaha arrived at the hospital, I took photos of my wrecked face, and we waited for the admissions process to move forward. She liked the nurse as much as I did.
I was put into an ER room, and Omaha went back to her hotel, utterly freaked out, as emotionally wrecked as I was. Eventually I was moved to a standard hospital bedroom, where I had a roommate and a very loud (65dB according to the sketchy sound meter on my phone)
Corsi-Rosenthall box. And it was friggin’ cold, but viral infections always wreck my ability to manage my internal temperature. He also kept the TV on all night long, and he stims; I can’t see him through the curtain separating our spaces, but he claps, he slaps himself, he whoops, he randomly outbursts in laughter or just random words, like a light case of Tourette’s syndrome.
And I was here for just “observation.” They would take my blood every 12 hours to make sure the hemoglobin levels stayed the same.
And I settled in for boredom. My beloved Omaha brought me my bag the next day with my books, my laptop, my chargers, my headphones, and my earlplugs! I was equipped for a long intellectual dry spell. Blood was drawn, meals were delivered.
Early on, there was some discussion as to whether or not the damage to my insides was caused by the fall or by COVID directly. The new trauma doctor, a no-nonsense woman of the highly competent stripe, told me that the trauma team had concluded it was a COVID complication. Again, research skills, ADHD and an internet connection, and I found a case study that matches mine:
Unexpected tendency to bleeding in COVID-19 patients: A case of spontaneous retroperitoneal hematoma. Healthy woman, no comorbidities, no suspect medications, 47 years old. I had tenderness in the left anterior abdomen, hers was in her back. I caught mine earlier than she did, so I did not need a transfusion. It took three months for her body to clear all that blood out of her peritoneal cavity.
More to come…